149 Physical Changes of Aging
Martha Lally; Suzanne Valentine-French; and Dinesh Ramoo
The Baltimore Longitudinal Study on Aging (BLSA) (National Institute on Aging, 2011b) began in 1958 and has traced the aging process in 1,400 people from ages twenty to ninety. Researchers from the BLSA have found that the aging process varies significantly from individual to individual and from one organ system to another. However, some key generalizations can be made, including heart muscles thickening with age, arteries becoming less flexible, and lung capacity diminishing. Kidneys become less efficient in removing waste from the blood, and the bladder loses its ability to store urine. Brain cells also lose some functioning, but new neurons can also be produced. Many of these changes are determined by genetics, lifestyle, and disease. Below are some of the other changes that occur in late adulthood.
Body changes: Everyone’s body shape changes naturally as they age. According to the National Library of Medicine (2014), after age thirty people tend to lose lean tissue, and some of the cells of the muscles, liver, kidney, and other organs are lost. Tissue loss reduces the amount of water in your body and bones may lose some of their minerals and become less dense (a condition called osteopenia in the early stages and osteoporosis in the later stages). The amount of body fat goes up steadily after age thirty, and older individuals may have almost one third more fat compared to when they were younger. Fat tissue builds up toward the centre of the body, including around the internal organs.
Skin and hair: With age, skin becomes thinner and less elastic, has less fat, and no longer looks plump and smooth. Veins and bones can be seen more easily and scratches, cuts, and bumps can take longer to heal. Years exposed to the sun may lead to wrinkles, dryness, age spots, and cancer. Older people may bruise more easily, and it can take longer for these bruises to heal. Some medicines or illnesses may also cause bruising. Gravity can cause skin to sag and wrinkle, and smoking can wrinkle the skin. Also seen in older adults are age spots, previously called “liver spots.” They look like flat, brown spots and are often caused by years in the sun. Skin tags are small, usually flesh-coloured growths of skin that have a raised surface. They become common as people age, especially for women, but both age spots and skin tags are harmless (National Institute on Aging, 2015f).
Nearly everyone has hair loss as they age, and the rate of hair growth slows down as many hair follicles stop producing new hairs. The loss of pigment and subsequent greying that began in middle adulthood continues in late adulthood.

Sarcopenia: A natural part of aging, sarcopenia is the loss of muscle tissue. Sarcopenia is most noticeable in men, and physically inactive people can lose as much as 3 to 5 percent of their muscle mass each decade after age thirty, but even when active muscle loss still occurs (WebMD, 2016). Symptoms include a loss of stamina and weakness, which can decrease physical activity and subsequently further shrink muscles. Sarcopenia typically happens faster around age seventy-five, but it may also speed up as early as sixty-five or as late as eighty. Factors involved in sarcopenia include a reduction in nerve cells responsible for sending signals to the muscles from the brain to begin moving, a decrease in the ability to turn protein into energy, and not receiving enough calories or protein to sustain adequate muscle mass. Any loss of muscle is important because it lessens strength and mobility, and sarcopenia is a factor in frailty and the likelihood of falls and fractures in older adults. Maintaining strong leg and heart muscles are important for independence. Weightlifting, walking, swimming, or engaging in other cardiovascular exercises can help strengthen the muscles and prevent atrophy.

Height and weight: The tendency to become shorter as one ages occurs among all races and both sexes. Height loss is related to aging changes in the bones, muscles, and joints. People typically lose almost one-half inch every ten years after age forty, and height loss is even more rapid after age seventy. A total of 1 to 3 inches in height is lost with aging. Changes in body weight vary for men and woman. Men often gain weight until about age fifty-five, and then begin to lose weight later in life, possibly related to a drop in the male sex hormone testosterone. Women usually gain weight until age sixty-five, and then begin to lose weight. Weight loss later in life occurs partly because fat replaces lean muscle tissue, and fat weighs less than muscle. Diet and exercise are important factors in weight changes in late adulthood (National Library of Medicine, 2014).
Sensory Changes in Late Adulthood
Vision: In late adulthood, all the senses show signs of decline, especially among the oldest-old. In the last chapter, you read about the visual changes that were beginning in middle adulthood, such as presbyopia, dry eyes, and problems seeing in dimmer light. By later adulthood these changes are much more common. Three serious eyes diseases are more common in older adults: cataracts, macular degeneration, and glaucoma. Only the first can be effectively cured in most people.
Cataracts are a clouding of the lens of the eye. The lens of the eye is made up of mostly water and protein. The protein is precisely arranged to keep the lens clear, but with age some of the protein starts to clump. As more of the protein clumps together the clarity of the lens is reduced. While some adults in middle adulthood may show signs of cloudiness in the lens, the area affected is usually small enough to not interfere with vision. More people have problems with cataracts after age sixty (National Institutes of Health, 2014b) and by age seventy-five, 70 percent of adults will have problems with cataracts (Boyd, 2014). Cataracts also cause a discolouration of the lens, tinting it more yellow and than brown, which can interfere with the ability to distinguish colours such as black, brown, dark blue, or dark purple.
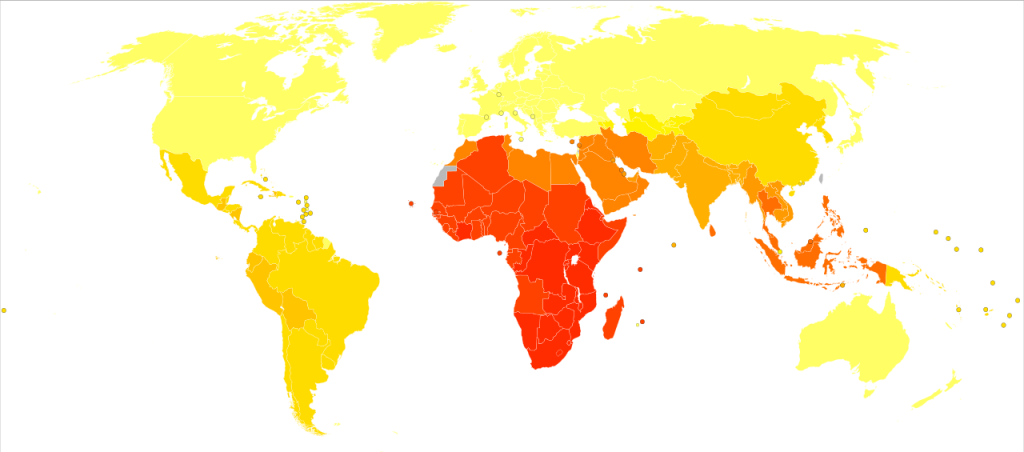
 Figure 9.15: Disability-adjusted life years for cataracts per 100,000 inhabitants in 2004
Figure 9.15: Disability-adjusted life years for cataracts per 100,000 inhabitants in 2004
Risk factors besides age include certain health problems (such as diabetes, high blood pressure, and obesity), behavioural factors (such as smoking), other environmental factors (such as prolonged exposure to ultraviolet sunlight, previous trauma to the eye, long-term use of steroid medication), and a family history of cataracts (National Eye Institute, 2016a; Boyd, 2014). Cataracts are treated by removing and replacing the lens of the eye with a synthetic lens. In developed countries, such as the United States, cataracts can be easily treated with surgery. However, in developing countries, access to such operations are limited, making cataracts the leading cause of blindness in late adulthood in developing nations (Resnikoff, Pascolini, Mariotti, and Pokharel, 2004). As shown in Figure 9.15, areas of the world with limited medical treatment for cataracts often have people living more years with a serious disability. For example, of those living in the darkest red colour on the map, more than 990 out of 100,00 people have a shortened lifespan due to the disability caused by cataracts.
Older adults are also more likely to develop age-related macular degeneration, which is the loss of clarity in the centre field of vision due to the deterioration of the macula, the centre of the retina. Macular degeneration does not usually cause total vision loss, but the loss of the central field of vision can greatly impair day-to-day functioning. There are two types of macular degeneration: dry and wet. The dry type is the most common form and occurs when tiny pieces of a fatty protein called drusen form beneath the retina. Eventually the macular becomes thinner and stops working properly (Boyd, 2016). About 10 percent of people with macular degeneration have the wet type, which causes more damage to their central field of vision than the dry form. This form is caused by an abnormal development of blood vessels beneath the retina. These vessels may leak fluid or blood, causing more rapid loss of vision than the dry form.
The risk factors for macular degeneration include: smoking, which doubles your risk (National Institutes of Health, 2015a); race, as it is more common among Caucasians than African Americans or Hispanics/Latinos; high cholesterol; and a family history of macular degeneration (Boyd, 2016). At least twenty different genes have been related to this eye disease, but there is no simple genetic test to determine your risk, despite claims by some genetic testing companies (National Institutes of Health, 2015a). At present, there is no effective treatment for the dry type of macular degeneration. Some research suggests that certain patients may benefit from a cocktail of certain antioxidant vitamins and minerals, but the results are mixed at best. They are not a cure for the disease nor will they restore the vision that has been lost. This “cocktail” can slow the progression of visual loss in some people (Boyd, 2016; National Institutes of Health, 2015a). For the wet type, medications that slow the growth of abnormal blood vessels and surgery, such as laser treatment to destroy the abnormal blood vessels, may be used. Only 25 percent of those with the wet version may see improvement with these procedures (Boyd, 2016).
A third vision problem that increases with age is glaucoma, which is the loss of peripheral vision, frequently due to a buildup of fluid in eye that damages the optic nerve. As you age, the pressure in the eye may increase causing damage to the optic nerve. The exterior of the optic nerve receives input from retinal cells on the periphery, and as glaucoma progresses more and more of the peripheral visual field deteriorates toward the central field of vision. In the advanced stages of glaucoma, a person can lose their sight. Fortunately, glaucoma tends to progress slowly (National Eye Institute, 2016b).


Figure 9.16: Normal vision vs. cataracts, macular degeneration, and glaucoma
Glaucoma is the most common cause of blindness in the US (National Eye Institute, 2016b). African Americans over age forty, and everyone else over age sixty have a higher risk for glaucoma. Those with diabetes and with a family history of glaucoma also have a higher risk (Owsley et al., 2015). There is no cure for glaucoma, but its rate of progression can be slowed, especially with early diagnosis. Routine eye exams to measure eye pressure and examination of the optic nerve can detect both the risk and presence of glaucoma (National Eye Institute, 2016b). Those with elevated eye pressure are given medicated eye drops. Reducing eye pressure lowers the risk of developing glaucoma or slows its progression in those who already have it.
Hearing: As you read in chapter eight, our hearing declines both in terms of the frequencies of sound we can detect and the intensity of sound needed to hear as we age. These changes continue in late adulthood. Almost 1 in 4 adults aged sixty-five to seventy-four and 1 in 2 aged seventy-five and older have disabling hearing loss (National Institutes of Health, 2016). Table 9.4 lists some common signs of hearing loss (adapted from National Institute on Aging, 2015c).
|
|
|
|
|
|
|
Presbycusis is a common form of hearing loss in late adulthood that results in a gradual loss of hearing. It runs in families and affects hearing in both ears (National Institute on Aging, 2015c). Older adults may also notice tinnitus, a ringing, hissing, or roaring sound in the ears. The exact cause of tinnitus is unknown, although it can be related to hypertension and allergies. It may come and go or persist and get worse over time (National Institute on Aging, 2015c). The incidence of both presbycusis and tinnitus increase with age and males have higher rates of both around the world (McCormak, Edmondson-Jones, Somerset, and Hall, 2016).
Your auditory system has two jobs: to help you to hear and to help you maintain balance. Your balance is controlled by the brain receiving information from the shifting of hair cells in the inner ear about the position and orientation of the body. With age, this function of the inner ear declines, which can lead to problems with balance when sitting, standing, or moving (Martin, 2014).
Taste and smell: Our sense of taste and smell are part of our chemical sensing system. Our sense of taste, or gustation, appears to age well. Normal taste occurs when molecules that are released by chewing food stimulate taste buds along the tongue, the roof of the mouth, and in the lining of the throat. These cells send messages to the brain, where specific tastes are identified. After age fifty we start to lose some of these sensory cells. Most people do not notice any changes in taste until ones sixties (National Institutes of Health: Senior Health, 2016b). Given that the loss of taste buds is very gradual, even in late adulthood, many people are often surprised that their loss of taste is most likely the result of a loss of smell.
| Presbysomia | Smell-loss due to aging |
| Hyposmia | Loss of only certain odours |
| Anosmia | Total loss of smell |
| Dysomia | Change in the perception of odours where familiar odours are distorted |
| Phantosmia | Smelling odours that are not present |
Our sense of smell, or olfaction, decreases more with age, and problems with the sense of smell are more common in men than in women. Almost 1 in 4 men in their sixties have a disorder with the sense of smell, while only 1 in 10 women do (National Institutes of Health: Senior Health, 2016b). This loss of smell due to aging is called presbysomia. Olfactory cells are located in a small area high in the nasal cavity. These cells are stimulated by two pathways: when we inhale through the nose, or via the connection between the nose and the throat when we chew and digest food. It is a problem with this second pathway that explains why some foods such as chocolate or coffee seem tasteless when we have a head cold. There are several types of loss of smell. Total loss of smell, or anosmia, is extremely rare (see Table 9.5 for types of smell disorders, adapted from National Institutes of Health: Senior Health, 2016a).
Problems with our chemical senses can be linked to other serious medical conditions such as Parkinson’s, Alzheimer’s, or multiple sclerosis (National Institutes of Health: Senior Health, 2016a). Any sudden change should be checked out. Loss of smell can change a person’s diet, with either a loss of enjoyment of food and eating too little for balanced nutrition, or adding sugar and salt to foods that are becoming blander to the palate.
Touch: Research has found that with age, people may experience reduced or changed sensations of vibration, cold, heat, pressure, or pain (Martin, 2014). Many of these changes are also aligned with a number of medical conditions that are more common among the elderly, such as diabetes. However, there are changes in the touch sensations among healthy older adults. The ability to detect changes in pressure have been shown to decline with age, with it being more pronounced by one’s sixties and diminishing further with advanced age (Bowden and McNelty, 2013). Yet, there is considerable variability, with almost 40 percent showing sensitivity that is comparable to younger adults (Thornbury and Mistretta, 1981). However, the ability to detect the roughness/smoothness or hardness/softness of an object shows no appreciable change with age (Bowden and McNulty, 2013). Those who show increasing insensitivity to pressure, temperature, or pain are at risk for injury (Martin, 2014).
Pain: According to Molton and Terrill (2014), approximately 60 to 75 percent of people over the age of sixty-five report at least some chronic pain, and this rate is even higher for those individuals living in nursing homes. Although the presence of pain increases with age, older adults are less sensitive to pain than younger adults (Harkins, Price, and Martinelli, 1986).

Farrell (2012) looked at research studies that included neuroimaging techniques involving older people who were healthy and those who experienced a painful disorder. Results indicated that there were age-related decreases in brain volume in those structures involved in pain. Especially noteworthy were changes in the prefrontal cortex, brainstem, and hippocampus. Women are more likely to identify feeling pain than men (Tsang et al., 2008). Women have fewer opioid receptors in the brain, and women also receive less relief from opiate drugs (Garrett, 2015). Because pain serves an important indicator that there is something wrong, a decreased sensitivity to pain in older adults is a concern because it can conceal illnesses or injuries requiring medical attention.
Media Attributions
- Figure 9 15 © Lokal_Profil is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9 15 legend © Dinesh Ramoo is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9 16a © National Institutes of Health is licensed under a Public Domain license
- Figure 9 16b © National Institutes of Health is licensed under a Public Domain license
- Figure 9 16c © National Institutes of Health is licensed under a Public Domain license
- Figure 9 16d © National Institutes of Health is licensed under a Public Domain license
- Figure 9 17 © Ian Furst is licensed under a CC BY-SA (Attribution ShareAlike) license

