
Sudden unexpected infant death (SUID): Each year in the United States, there are about 3,500 SUIDs. These deaths occur among infants less than one year old and have no immediately obvious cause (CDC, 2015). The three commonly reported types of SUID are:
- Sudden infant death syndrome (SIDS): SIDS is identified when the death of a healthy infant occurs suddenly and unexpectedly, and medical and forensic investigation findings (including an autopsy) are inconclusive. SIDS is the leading cause of death in infants one to twelve months old, and approximately 1,500 infants died of SIDS in 2013 (CDC, 2015). Because SIDS is diagnosed when no other cause of death can be determined, possible causes of SIDS are regularly researched. One leading hypothesis suggests that infants who die from SIDS have abnormalities in the area of the brainstem responsible for regulating breathing (Weekes-Shackelford and Shackelford, 2005).
- Unknown cause: Sometimes the sudden death of an infant less than one year of age cannot be explained because a thorough investigation was not conducted and cause of death could not be determined.
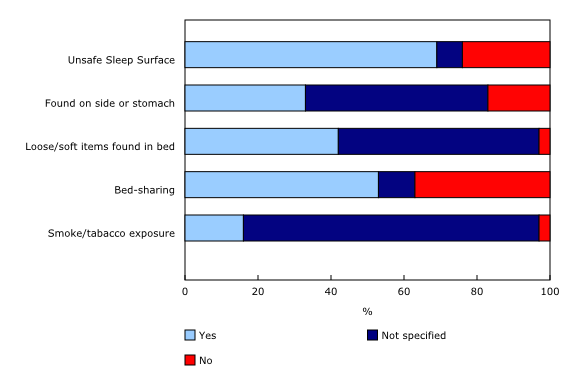
- Accidental suffocation and strangulation in bed: Reasons for accidental suffocation include suffocation by soft bedding, another person rolling on top of or against the infant while sleeping, an infant being wedged between two objects such as a mattress and wall, and strangulation such as when an infant’s head and neck become caught between crib railings. The percentages of infants who died based on various risk factors are listed in Figure 3.5.
As can be seen in the below graph (Figure 3.6), the combined SUID death rate declined considerably following the release of the American Academy of Pediatrics safe sleep recommendations in 1992, which advocated that infants be placed for sleep on their backs (non-prone position). These recommendations were followed by a major Back to Sleep Campaign in 1994. However, accidental suffocation and strangulation in bed mortality rates remained unchanged until the late 1990s. In 1998, death rates from accidental suffocation and strangulation in bed actually started to increase, and they reached the highest rate at 20.8 deaths per 100,000 live births in 2013.
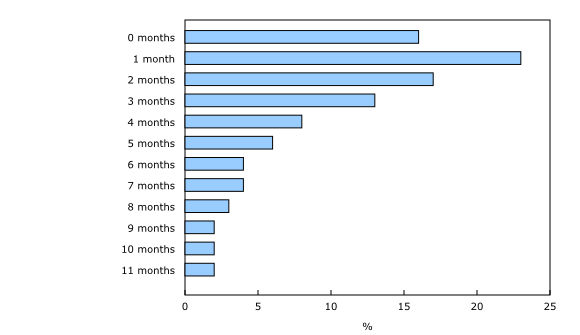
Should Infants be Sharing the Bed With Parents?Colvin, Collie-Akers, Schunn and Moon (2014) analyzed a total of 8,207 deaths from twenty-four states during 2004–2012 that were contained in the National Center for the Review and Prevention of Child Deaths Case Reporting System, a database of death reports from state child-death review teams. The results indicated that younger victims (birth to three months) were more likely to die by bed-sharing and sleeping in an adult bed/on a person. A higher percentage of older victims (four months to one year) rolled into objects in the sleep environment and changed position from side/back to prone. Carpenter et al. (2013) compared infants who died of SIDS with a matched control and found that infants younger than three months old who slept in bed with a parent were five times more likely to die of SIDS compared to babies who slept separately from the parents, but were still in the same room. They concluded that bed sharing, even when the parents do not smoke or take alcohol or drugs, increases the risk of SIDS. However, when combined with parental smoking and maternal alcohol consumption and/or drug use, risks associated with bed sharing greatly increased.
 The two studies discussed above were based on US statistics. What about the rest of the world? Co-sleeping occurs in many cultures, primarily because of a more collectivist perspective that encourages a close parent-child bond and interdependent relationship (Morelli, Rogoff, Oppenheim, and Goldsmith, 1992). In countries where co-sleeping is common, however, parents and infants typically sleep on floor mats and other hard surfaces which minimize the suffocation that can occur with bedding and mattresses (Nelson, Schiefenhoevel, and Haimerl, 2000). |

