- Timing of the exposure: Structures in the body are vulnerable to the most severe damage when they are forming. If a substance is introduced during a particular structure’s critical period of development, the damage to that structure may be greater. For example, the ears and arms reach their critical periods at about six weeks after conception. If a mother exposes the embryo to certain substances during this period, the arms and ears may be malformed.
- Amount of exposure: Some substances are not harmful unless the amounts reach a certain level. The critical level depends in part on the size and metabolism of the mother.
- Number of teratogens: Fetuses exposed to multiple teratogens typically have more problems than those exposed to only one.
- Genetics: Genetic makeup also plays a role on the impact a particular teratogen might have on the child. This is suggested by fraternal twins exposed to the same prenatal environment, but who do not experience the same teratogenic effects. The genetic makeup of the mother can also have an effect; some mothers may be more resistant to teratogenic effects than others.
- Sex: Males are more likely to experience damage due to teratogens than females. It is believed that the Y chromosome, which contains fewer genes than the X, may have an impact.
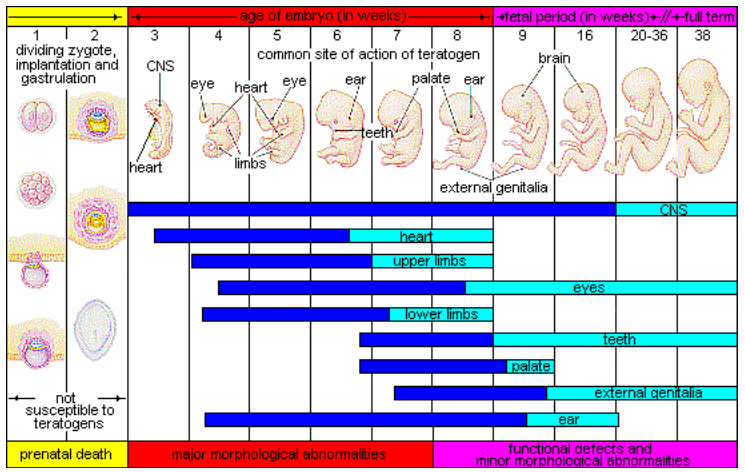
Figure 2.9 illustrates the timing of teratogen exposure and the types of structural defects that can occur during the prenatal period.
Alcohol: One of the most commonly used teratogens is alcohol, and because half of all pregnancies in the United States are unplanned, it is recommended that women of child-bearing age take great caution against drinking alcohol when not using birth control or when pregnant (CDC, 2005). Alcohol use during pregnancy is the leading preventable cause of intellectual disabilities in children in the United States (Maier & West, 2001). Alcohol consumption, particularly during the second month of prenatal development but at any point during pregnancy, may lead to neurocognitive and behavioural difficulties that can last a lifetime. Binge drinking (five or more drinks on a single occasion) or consuming seven or more drinks during a single week place a child at risk.
In extreme cases, alcohol consumption during pregnancy can lead to fetal death, but also can result in fetal alcohol spectrum disorders (FASD), which is an umbrella term for the range of effects that can occur due to alcohol consumption during pregnancy (March of Dimes, 2016a). The most severe form of FASD is fetal alcohol syndrome (FAS). Children with FAS share certain physical features such as flattened noses, small eye holes, and small heads (see Figure 2.10). Cognitively, these children have poor judgment, poor impulse control, higher rates of ADHD, learning issues, and lower IQ scores. These developmental problems and delays persist into adulthood (Streissguth, Barr, Kogan, and Bookstein, 1996) and can include criminal behaviour, psychiatric problems, and unemployment (CDC, 2016a). Based on animal studies, it has been hypothesized that a mother’s alcohol consumption during pregnancy may predispose her child to like alcohol (Youngentob, Molina, Spear, and Youngentob, 2007).

Tobacco: Another widely used teratogen is tobacco. According to Tong et al. (2013) in conjunction with the Centers for Disease Control and Prevention, data from 27 sites in 2010, representing 52 percent of live births, showed that among women with recent live births:
- about 23 percent reported smoking in the three months prior to pregnancy;
- almost 11 percent reported smoking during pregnancy;
- more than half (54.3 percent) reported that they quit smoking by the last three months of pregnancy; and
- almost 16 percent reported smoking after delivery.
When comparing the ages of women who smoked, researchers found:
- 13.6 percent of women aged <20 smoked during pregnancy;
- 17.6 percent of women aged 20–24 smoked during pregnancy;
- 8.8 percent of women aged 25–34 smoked during pregnancy; and
- 5.7 percent of women aged ≥35 smoked during pregnancy.
The findings among racial and ethnic groups indicated that smoking during pregnancy was highest among American Indians/Alaska Natives (26.0 percent) and lowest among Asians/Pacific Islanders (2.1 percent).
When a pregnant woman smokes, the fetus is exposed to dangerous chemicals including nicotine, carbon monoxide, and tar, which reduce the amount of oxygen available to the fetus. Oxygen is important for overall growth and development. Tobacco use during pregnancy has been associated with low birth weight, ecotopic pregnancy (fertilized egg implants itself outside of the uterus), placenta previa (placenta lies low in the uterus and covers all or part of the cervix), placenta abruption (placenta separates prematurely from the uterine wall), pre-term delivery, stillbirth, fetal growth restriction, sudden infant death syndrome (SIDS), birth defects, learning disabilities, and early puberty in girls (Center for Disease Control, 2015d). A woman being exposed to secondhand smoke during pregnancy has also been linked to low-birth-weight infants.
Prescription/over-the-counter drugs: About 70 percent of pregnant women take at least one prescription drug (March of Dimes, 2016e). A woman should not be taking any prescription drug during pregnancy unless it was prescribed by a healthcare provider who knows she is pregnant. Some prescription drugs can cause birth defects, problems in overall health, and problems in the development of the fetus. Over-the-counter drugs are also a concern during the prenatal period because they may cause certain health problems. For example, the pain reliever ibuprofen can cause serious blood flow problems to the fetus during the last three months.

Illicit drugs: Common illicit drugs include cocaine, ecstasy and other club drugs, heroin, marijuana, and prescription drugs that are abused. It is difficult to completely determine the effects of a particular illicit drug on a developing child because most mothers who use them use more than one substance and have other unhealthy behaviours. These include smoking, drinking alcohol, not eating healthy meals, and being more likely to get a sexually transmitted disease. However, several problems seem clear. The use of cocaine is connected with low birth weight, stillbirths, and spontaneous abortion. Heavy marijuana use is associated with problems in brain development (March of Dimes, 2016c). If a baby’s mother used an addictive drug during pregnancy that baby can get addicted to the drug before birth and go through drug withdrawal after birth, also known as neonatal abstinence syndrome (March of Dimes, 2015d). Other complications of illicit drug use include premature birth, smaller-than-normal head size, birth defects, heart defects, and infections. Additionally, babies born to mothers who use drugs may have problems later in life, including learning and behavioural difficulties, slower than normal growth, and sudden infant death syndrome (SIDS). Children of substance-abusing parents are also considered at high risk for a range of biological, developmental, academic, and behavioural problems, including developing substance-abuse problems of their own (Conners, et al., 2003).
Box 2.3: Should Women Who Use Drugs During Pregnancy Be Arrested and Jailed?Women who use drugs or alcohol during pregnancy can cause serious lifelong harm to their child. Some people have advocated for mandatory screenings for women who are pregnant and have a history of drug abuse, and if the women continue using, to arrest, prosecute, and incarcerate them (Figdor and Kaeser, 1998). Canada does not have any laws specific to substance abuse during pregnancy. This policy was tried in Charleston, South Carolina twenty years ago. The policy was called the Interagency Policy on Management of Substance Abuse During Pregnancy and had disastrous results. The Interagency Policy applied to patients attending the obstetrics clinic at the Medical University of South Carolina, which primarily serves patients who are indigent or on Medicaid. It did not apply to private obstetrical patients. The policy required patient education about the harmful effects of substance abuse during pregnancy. A statement also warned patients that protection of unborn and newborn children from the harms of illegal drug abuse could involve the Charleston police, the Solicitor of the Ninth Judicial Court, and the Protective Services Division of the Department of Social Services (DSS) (Jos, Marshall, and Perlmutter, 1995, pp. 120–121). This policy seemed to deter women from seeking prenatal care, deterred them from seeking other social services, and was applied solely to low-income women, resulting in lawsuits. The program was canceled after five years, during which forty-two women were arrested. A federal agency later determined that the program involved human experimentation without the approval and oversight of an institutional review board. In July 2014, Tennessee enacted a law that allows women who illegally use a narcotic drug while pregnant to be prosecuted for assault if her infant is harmed or born addicted to the drug (National Public Radio, 2015). According to the National Public Radio report, a baby is born dependent on a drug every thirty minutes in Tennessee, which is a rate three times higher than the national average. However, since the law took effect, the number of babies born having drug withdrawal symptoms has not diminished. Research shows that arrests and detentions have not resulted in prompt or appropriate treatment and care and are a violation of the constitutional rights of pregnant women (Uberoi et al., 2013; Paltrow and Falvin, 2013). Critics contend that the criminal justice system should not be involved in what is considered a healthcare problem. The Society of Obstetricians and Gynecologists of Canada support healthcare providers in addressing substance use with women in the perinatal period. What do you think? Is the issue of mothers using illicit drugs a legal concern or a medical concern? |
Pollutants: There are more than 83,000 chemicals used in the United States with little information on their effects during pregnancy (March of Dimes, 2016b). An environmental pollutant of significant concern is lead poisoning, which is connected with low birth weight and slowed neurological development. The chemicals in certain pesticides are also potentially damaging and may lead to birth defects, learning problems, low birth weight, miscarriage, and premature birth (March of Dimes, 2014). Prenatal exposure to bisphenol A (BPA), a chemical commonly used in plastics and food and beverage containers, may disrupt the action of certain genes contributing to certain birth defects (March of Dimes, 2016b). Radiation is another environmental hazard. If a mother is exposed to radiation, it can get into her bloodstream and pass through the umbilical cord to the baby. Radiation can also build up in body areas close to the uterus, such as the bladder. Exposure to radiation can slow the baby’s growth, cause birth defects, affect brain development, cause cancer, and result in a miscarriage. Mercury, a heavy metal, can cause brain damage and affect the baby’s hearing and vision. This is why women are cautioned about the amount and type of fish they consume during pregnancy.

Toxoplasmosis: The tiny parasite, Toxoplasma gondii, causes an infection called toxoplasmosis. According to the March of Dimes (2012d), Toxoplasma gondii infects more than 60 million people in the United States. A healthy immune system can keep the parasite at bay producing no symptoms, so most people do not know they are infected. As routine prenatal screening frequently does not test for the presence of this parasite, pregnant women may want to talk to their healthcare provider about being tested. Toxoplasmosis can cause premature birth, stillbirth, and can result in birth defects to the eyes and brain. While most babies born with this infection show no symptoms, 10 percent may experience eye infections, enlarged liver and spleen, jaundice, and pneumonia. To avoid being infected, women should avoid eating undercooked or raw meat and unwashed fruits and vegetables, touching cooking utensils that touched raw meat or unwashed fruits and vegetables, and touching cat feces, soil, or sand. If women think they may have been infected during pregnancy, they should have their baby tested.
Sexually transmitted diseases: Gonorrhea, syphilis, and chlamydia are sexually transmitted infections that can be passed to the fetus by an infected mother. Mothers should be tested as early as possible to minimize the risk of spreading these infections to their unborn children. Additionally, the earlier the treatment begins, the better the health outcomes for mother and baby (CDC, 2016d). Sexually transmitted diseases (STDs) can cause premature birth, premature rupture of the amniotic sac, an ectopic pregnancy, birth defects, miscarriage, and still births (March of Dimes, 2013). Most babies become infected with STDs while passing through the birth canal during delivery, but some STDs can cross the placenta and infect the developing fetus.
Human immunodeficiency virus (HIV): One of the most potentially devastating teratogens is HIV. HIV and acquired immune deficiency syndrome (AIDS) are leading causes of illness and death in the United States (Health Resources and Services Administration, 2015). One of the main ways children under age 13 become infected with HIV is via mother-to-child transmission of the virus prenatally, during labor, or by breastfeeding (CDC, 2016c). There are some measures that can be taken to lower the chance the child will contract the disease. HIV-positive mothers who take antiviral medications during their pregnancy greatly reduce the chance of passing the virus to the fetus. The risk of transmission is less than 2 percent; in contrast, it is 25 percent if the mother does not take antiretroviral drugs (CDC, 2016b). However, the long-term risks of prenatal exposure to the medication are not known. It is recommended that women with HIV deliver the child by Caesarean section, and that after birth they avoid breastfeeding.
German measles (or rubella): Rubella, also called German measles, is an infection that causes mild flu-like symptoms and a rash on the skin. However, only half of children infected have these symptoms, while others have no symptoms (March of Dimes, 2012a). Rubella has been associated with a number of birth defects. If the mother contracts the disease during the first three months of pregnancy, damage can occur in the eyes, ears, heart, or brain of the unborn child. Deafness is almost certain if the mother has German measles before the eleventh week of prenatal development, and brain damage is also possible at this stage. Women in the United States are much less likely to be afflicted with rubella, because most women have received childhood vaccinations that protect from the disease.

