151 Chronic Conditions
Martha Lally; Suzanne Valentine-French; and Dinesh Ramoo
Chronic illnesses are illnesses that are ongoing, generally incurable conditions that require continuing medical attention and affect daily life. As individuals live longer, diseases that affect older individuals will become more prevalent, and the burden of chronic illness grows with age. Less than 50 percent of adults aged fifty to sixty-four have a chronic condition, yet 90 percent aged seventy-five and up do (Cohen, 2011). Older women are more likely to have a chronic condition than are older men (83 vs. 88 percent) (Centers for Disease Control and Prevention, 2009). Table 9.6 lists the percentage of older adults who have certain chronic illnesses based on the National Health Survey conducted in 2014. Other studies place the figure of diabetes in older adults at 26 percent (Centers for Disease Control and Prevention, 2014).
| High Cholesterol | 58.2 |
|---|---|
| Hypertension | 56.7 |
| Arthritis | 48.7 |
| Cancer | 23.1 |
| Diabetes | 20.5 |
| Heart disease | 17.9 |
| Ulcers | 11.3 |
| Stroke | 7.2 |
| Asthma | 6.9 |
| Kidney disease | 5.1 |
| Chronic bronchitis | 5.0 |
| Emphysema | 4.0 |
Cancer and major cardiovascular disease: As discussed in chapter eight, cancer and cardiovascular disease are the overall leading causes of death, and their rates are especially high in middle and late adults. Table 9.7 identifies the percentages of deaths due to cancer and cardiovascular disease for selected age groups in 2013; the most recent year for data (Xu, Murphy, Kochanek, and Bastian, 2016).
| Age Groups | |||||
|---|---|---|---|---|---|
| 2013 Causes of Death | 45–54 | 55–64 | 65–74 | 75–84 | 85+ |
| Cancer | 6.4 | 13.7 | 24.9 | 24.5 | 12 |
| Major Cardiovascular Disease | 24.3 | 26.5 | 27.7 | 31.6 | 38.9 |
Cancer: Advancing age is a significant risk factor for cancer, with persons over sixty-five accounting for 60 percent of newly diagnosed cancer and 70 percent of all cancer deaths (Berger et al., 2006). Additionally, more than 70 percent of the mortality associated with many cancers, including prostate, bladder, colon, uterus, pancreas, stomach, rectum, and lung, occur in patients sixty-five and older. Other conditions that affect the elderly can occur with cancer, including anemia, coronary artery diseases, congestive heart failure, chronic obstructive pulmonary diseases, renal insufficiency, cerebrovascular diseases, neurovascular complications of diabetes mellitus, and arthritis that restricts mobility (Balducci and Extermann, 2000). Comorbidity will complicate treatment.
Balducci and Extermann (2000) examined several concerns of cancer treatment in the elderly. With aging, there is a decline in multiple organ systems that can adversely affect the ability of medications to treat the cancer. Chemotherapy has been found to compromise the cognitive function of those being treated for cancer, and it may further exacerbate dementia and elderly cognitive declines. Frail individuals, defined as having limited life expectancy and near-to-exhausted functional reserves, are also not considered candidates for more toxic forms of chemotherapy. With cancer, the prevalence and risk of malnutrition are higher, and diminished visual and hearing function makes elderly cancer patients more susceptible to environmental injury. Screening for depression is also recommended because depression is associated with weight loss and failure to thrive, and may reduce the motivation to receive treatment. Consequently, depression has been associated with decreased survival rates in the elderly. Due to the projected increase in the total number of older patients with cancer, it is recommended that physicians and caretakers have expertise in both oncology and geriatrics (Berger et al., 2006).
Heart disease: There are changes to the heart that happen with age, and some may increase a person’s risk of heart disease. These include stiffening blood vessels and valves, which may result in leaks or problems pumping blood out of the heart (National Institute on Aging, 2012). As previously stated, heart disease is the leading cause of death for those in late adulthood (Centers for Disease Control and Prevention, 2016b). There are different types of heart disease, and as already discussed in chapter eight, the most common is atherosclerosis, the buildup of fatty deposits or plaque in the walls of arteries. As plaque builds up, blood is unable to flow normally and bring oxygen throughout the body, including to the heart. Depending on where the buildup is, atherosclerosis can cause a heart attack, leg pain, or a stroke. However, atherosclerosis is not part of normal aging. Many of the problems older people have with their heart and blood vessels are caused by disease and not by aging. For example, an older heart can normally pump blood as strong as a younger heart, while a decrease in the ability to pump blood is caused by disease. Therefore, leading a heart-healthy lifestyle is most important to keeping one’s heart strong in late adulthood.
Arthritis: Arthritis and other rheumatic conditions are the most common cause of disability among US adults, and have been the most common cause of disability among US adults for the past fifteen years (National Institutes of Health: National Institute of Arthritis and Musculoskeletal and Skin Diseases, 2014). According to the National Institutes of Health, approximately 62 percent of adults with arthritis are sixty-five and older. Almost 1 in 2 older adults with arthritis have some degree of mobility limitation, such as climbing stairs, walking, and grasping objects. The pain and other limitations of arthritis can also increase the risk of depression and other forms of mental distress.
Osteoarthritis is the most common type of arthritis. “When the cartilage, the slick, cushioning surface on the ends of bones wears away, bone rubs against bone, causing pain, swelling and stiffness. Over time, joints can lose strength and pain may become chronic” (Arthritis Foundation, 2017, para 3). Common risk factors for osteoarthritis include genetics, obesity, age, previous injury, and other medical conditions.
Osteoporosis and kyphosis: Osteoporosis is a disease that thins and weakens bones to the point that they become fragile and break easily. After age fifty, 1 in 2 women and 1 in 4 men will experience an osteoporosis-related fracture in their lifetime, often leading to hip, spine, and wrist fractures (Dailey and Cravedi, 2006). Broken hips are a very serious problem as we age. They greatly increase the risk of death, especially during the year after they break (National Institutes of Health: Senior Health, 2015). In the US more than 53 million adults either already have osteoporosis or at a high risk due to low bone mass (National Institutes of Health: Senior Health, 2015). As bones weaken in the spine, adults gradually lose height and their posture becomes hunched over, which is called kyphosis. Over time, a bent spine can make it hard to walk or even sit up. Adults can prevent the loss of bone mass by eating a healthy diet with enough calcium and vitamin D, regularly exercising, limiting alcohol, and not smoking (National Osteoporosis Foundation, 2016).
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease in which the airways become damaged, making it difficult to breathe. COPD includes problems such as emphysema and chronic bronchitis (National Institutes of Health: Senior Health, 2013). COPD kills more than 120,000 people every year, making it one of the leading causes of death.
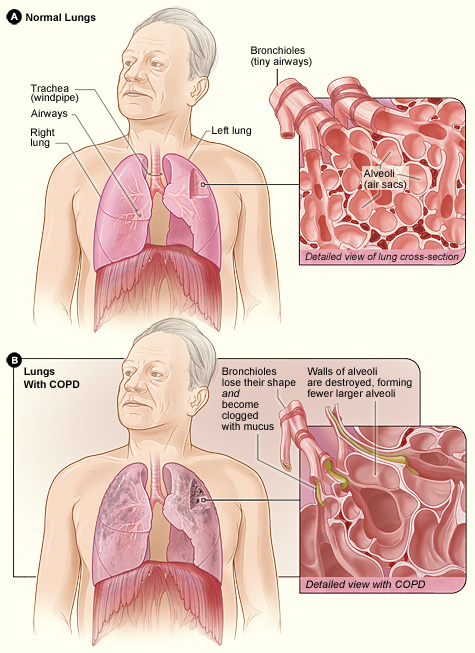
Figure 9.20 compares healthy to damaged lungs due to COPD. As COPD develops slowly, people may not notice the early signs, and may attribute the shortness of breath to age or lack of physical exercise. Most people are not diagnosed until midlife or late adulthood. There is no cure as the damage cannot be reversed. Treatments aim at slowing further damage.
Cigarette smoking is the leading cause of COPD, but other types of tobacco smoking, such as a pipe or cigar, can cause COPD, especially if the smoke is inhaled. Heavy or long-term exposure to secondhand smoke can also lead to COPD (National Institutes of Health: Senior Health, 2013). COPD can also occur in people who have long-term exposure to other environmental irritants, such as chemical fumes and dust from the environment and workplace.
About 1 in every 1,600 to 5,000 people have a risk for COPD because of a recessive genetic condition known as alpha-1 antitrypsin (AAT) deficiency (National Institutes of Health, 2011). AAT is a protein made in the liver that protects organs, especially the lungs, from the effects of other harmful proteins. In those with the genetic defect, the AAT protein created is the wrong shape and cannot leave the liver. This can lead to a heightened risk for lung disease, and even liver disease, as the excess of the AAT protein can lead to cirrhosis, which is a disease in which the liver becomes scarred and does not function properly. While some people with ATT deficiency are not affected and live a normal life, COPD is more likely to occur in such individuals if their lungs are exposed to environmental irritants.
Shingles: According to the National Institute on Aging (2015e), shingles is a disease that affects your nerves. Shingles is caused by the same virus as chicken pox, the varicella-zoster virus (VZV). After you recover from chickenpox, the virus continues to live in some of your nerve cells. It is usually inactive, and most adults live with VZV in their body and never get shingles. However, the virus will become active in 1 in 3 adults. Instead of causing chickenpox again, it produces shingles. A risk factor for shingles includes advanced age as people have a harder time fighting off infections as they get older. About half of all shingles cases are in adults age sixty or older, and the chance of getting shingles becomes much greater by age seventy. Other factors that weaken an individual’s ability to fight infections, such as cancer, HIV infections, or other medical conditions, can put one at a greater risk for developing shingles.

Shingles results in pain, burning, tingling, or itching in the affected area, as well as a rash and blisters. Typically, shingles develops only on one side of the body or face and in a small area rather than all over. Most cases of shingles last three to five weeks. After the shingles rash goes away, some people may be left with ongoing pain, called post-herpetic neuralgia (PHN), in the area where the rash had been (National Institute on Aging, 2015e). The older one is when getting shingles, the greater the chance of developing PHN. Some people with PHN find it hard to go about their daily activities, like dressing, cooking, and eating. They can also suffer from depression, anxiety, and sleeplessness. Medicines can help with pain, and usually PHN will disappear. Unfortunately, the blisters from shingles may become infected or leave a scar. Blisters near or in the eye can cause lasting eye damage or blindness. A brief paralysis of the face, hearing loss, and, very rarely, swelling of the brain (encephalitis) can also occur. There is a shingles vaccine recommended for those aged sixty and older. Shingles is not contagious, but one can catch chickenpox from someone with shingles.
Media Attributions
- Figure 9 19 © James Heilman, MD is licensed under a CC BY-SA (Attribution ShareAlike) license
- Figure 9 20 © National Heart Lung and Blood Institute is licensed under a Public Domain license
- Figure 9 21 © Gentgeen is licensed under a CC BY-SA (Attribution ShareAlike) license

